


Rh antigens, Rhesus Factor

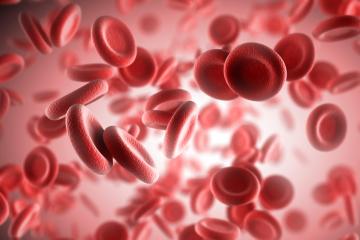
Rh antigens are explicitly expressed on the surface of red blood cells (RBCs) in humans and higher primates. Of more than 50 different components of the Rh blood group system, the D antigen, also known as Rho or Rho(D), is the most immunogenic. More than 90% of HDFN caused by Rh-incompatibility is attributed to antibodies against the D antigen. Therefore, the term Rh, such as Rh-incompatible or Rh-negative, refers to the Rho(D) antigen, and Rh is used interchangeably with D.
The gene for the D antigen is inherited in an autosomal dominant manner; persons with a single gene for the D antigen will have detectable antigen on their RBCs. 1,3 Therefore, the risk of Rh immunization depends on the frequency of the D gene in a given population, which differs among populations of different ethnic origins. 1
RH ANTIGENS, DATA
Approximately 50% of Rh-positive individuals are homozygous for the D gene. In a population of European descent, with a 15% frequency of Rh negative blood type, 12.8% of couplings will be of Rh-positive men with Rh-negative women (85% x 15%). In half of these pairs, the father will be homozygous for the D gene, and all fetuses will be Rh-positive. In the remaining half, the father will be heterozygous for the D gene and the probability of an Rh-positive fetus will be 50%. Therefore, the expected percentage of Rh-incompatible pregnancies this particular population is 9.6% (75% X 12.8%).
The public health ramifications of Rh antigens are enormous. The US National Vital Statistics Report estimates that there were 3,952,841 live births in 2012. The US Centers for Disease Control and Prevention (CDC) has reported that in 2012, there were a total of 699,202 reported abortions. Therefore, of approximately 4,650,000 pregnancies in the US in 2012, we can estimate that approximately 446,000 were Rh-incompatible (4,650,000 X 9.6%).
Maternal Rh immunization occurs when RBCs from the fetus, positive for the blood group factor Rh, cross the placenta into the maternal circulation during a fetal-maternal hemorrhage, or FMH. In 1939 Levine and Stetson described a case of a woman with type O blood who, following the delivery of a stillborn fetus with erythroblastosis fetalis, had a severe hemolytic reaction following a transfusion with her husband’s type O blood. Levine and co-workers correctly theorized that the development of maternal antibodies directed against the fetal RBC Rh antigens during one pregnancy may adversely affect subsequent pregnancies.
1. Rubin E, Farber JL. Developmental and genetic diseases. In:Rubin E, Farber JL, eds. Pathology. 2nd ed. Philadelphia, PA: J.B.Lippincott Company; 1994:255-8.
2. Prasad AS. Acquired hemolytic anemias. In: Bick RL, ed.Hematology, Clinical and Laboratory Practice. St Louis, MO:Mosby-Yearbook, Inc; 1993;1:391-6.
3. Turgeon ML. Hemolytic disease of the newborn. In: Turgeon ML, ed. Fundamentals of Immunohematology: Theory and Technique.Philadelphia, PA: Lea & Febiger; 1989: 321-43.
4. Levine P, Stetson RE. Unusual case of intragroup agglutination.JAMA. 1939;113:126-7.
5. Landsteiner K, Wiener AS. An agglutinable factor in human blood recognized by immune sera for rhesus blood. Proc SocExp Biol Med. 1940;43:223.
6. Levine P, Katzin EM, Burnham L. Isoimmunization in pregnancy: its possible bearing on the etiology of erythroblastosis fetalis. JAMA. 1941;116:825-7